Meet the Winners of the 2024 UCLA Health Equity Challenge

Four projects were recently selected as the winners of the 2024 Health Equity Challenge, which was sponsored by the UCLA Center for Health Policy Research (CHPR), The MolinaCares Accord, in collaboration with Molina Healthcare of California, and the California Health Care Foundation.
Launched in 2022, the Health Equity Challenge invites graduate students from any UCLA department or school to propose a project that would help address a health disparity in Los Angeles, San Bernardino, or Riverside counties. This year’s 15 finalists developed projects spanning everything from destigmatizing mental health care to training citizen scientists to breaking the homelessness-to-incarceration cycle to combatting food insecurity to improving health care for people who are unhoused. The winning proposals, which were chosen by an independent review committee, will receive $50,000 that the partnering community organization can use to implement the proposal. The students will also each receive $2,500 stipends.
The winning projects are:
Street Side Medicine Applications of Ultrasound: Using Point-of-Care Ultrasound to Screen for Heart Failure among People Experiencing Homelessness in Hollywood
Em Dickey
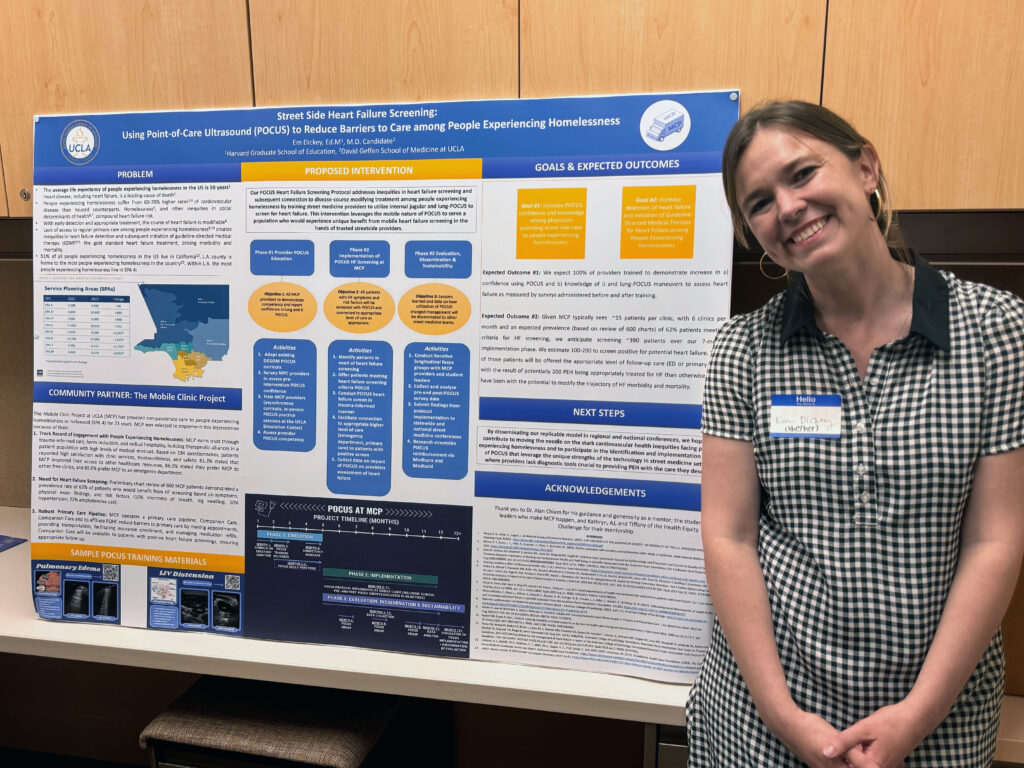
Community-based partner: UCLA Mobile Clinic Project
For her project, Em Dickey will bring point-of-care ultrasound technology to the volunteer health care providers who staff the UCLA Mobile Clinic, which has been operating in Hollywood offering free medical care for people experiencing homelessness for 25 years. Dickey said that this type of diagnostic screening tool will allow the clinic to identify early heart failure in patients experiencing homelessness.
She said she chose to focus her Health Equity Challenge project on expanding the range of care offered by the Mobile Clinic Project in part based on how she has observed doctors judge people experiencing homelessness. That lack of compassion contributes to why some people who most need medical attention don’t seek out health care, Dickey said.
“We also know that the quality of care we often provide on the streets is lower and we have fewer tools,” said Dickey, a medical student at the David Geffen School of Medicine at UCLA. “POCUS — point-of-care ultrasound — represents an exciting way to use that technology to bring care to people and specifically heart failure screening.”
Dickey chose to focus on using the technology for heart screening because it’s relatively easy to teach people how to use the devices to screen a person’s lungs and jugular for signs of heart failure, which could determine if you need to go to a primary care doctor or go to the emergency room.
“It’s a way to bring the quality of care that’s available to people in formal health care settings — so in clinics or hospitals — to the streets,” Dickey said. “More than anything I feel honored to be able to have brought more resources to an organization that works so tirelessly to serve unhoused community members.”
Power and Expertise of Peers with Lived Experience (PEoPLE): A Peer Specialist Pilot for a Jail Diversion and Housing Program
Dr. Sal Kamal
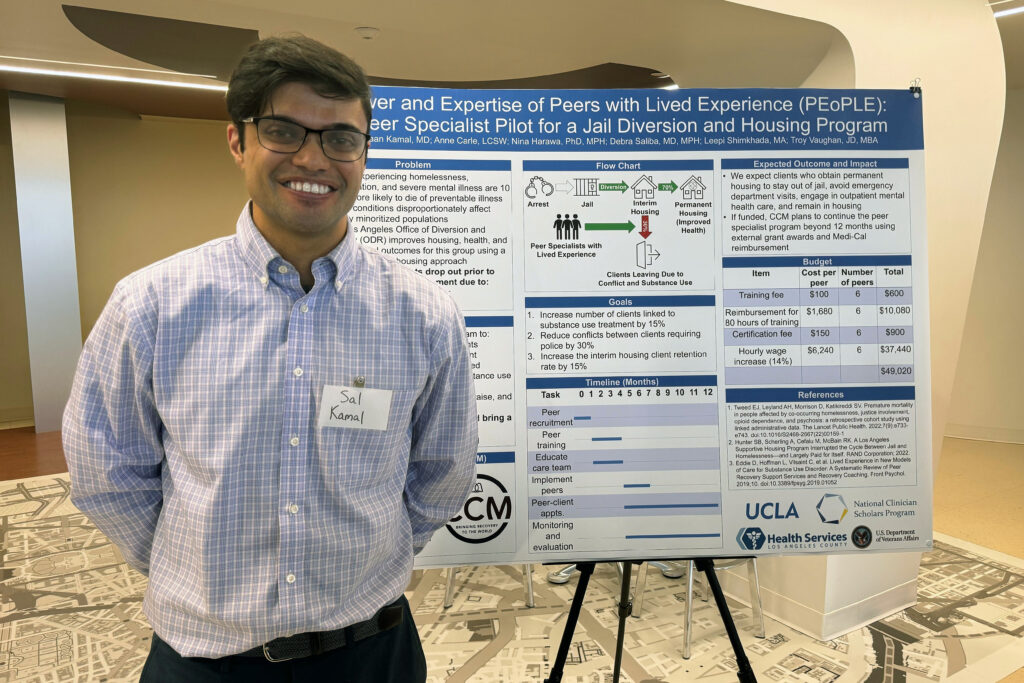
Community-based partner: Christ-Centered Ministries
Dr. Sal Kamal’s project will leverage the experiences, knowledge and empathy of people with lived experiences of incarceration and homelessness to strengthen existing programs offered by Christ-Centered Ministries that already serve these folks. The program works by diverting them out of jail and into housing with wraparound case management, mental health, and primary care services.
Kamal said he chose this as his Health Equity Challenge project because of what he observed in his clinical practice when he saw how important it was to gain an understanding of a patient’s experiences. He learned how following a typical doctor’s instructions like “make sure to take your meds as scheduled” is difficult when someone doesn’t have stable housing.
“I’m drawn to the patients that don’t have voice and don’t have power in our community,” said Kamal, who is an MS in Health Policy and Management student at the UCLA Fielding School of Public Health and a fellow of the UCLA National Clinician Scholars Program.
He noted that the people whose voices are so-often ignored are those experiencing homelessness or incarceration. “I realized through caring for them that pills don’t really help. What they need is housing and what they need is just relief from the carceral system in our country. So that’s what drew me to this idea, to this program.
“The largest untapped resource for this community to help them succeed, are people with lived experience, people that have been through the system that can connect with these people and really give them a fair shake” Kamal said. “If we partner with those folks and bring them to the front lines and to the top of organizations, it could really help all of us.”
MANTIS (Mental Wellbeing Approaches – Integrative and Traditional Chinese Medicine Igniting Self-Efficacy) for Chinese American Youths in the San Gabriel Valley
Michelle Ko
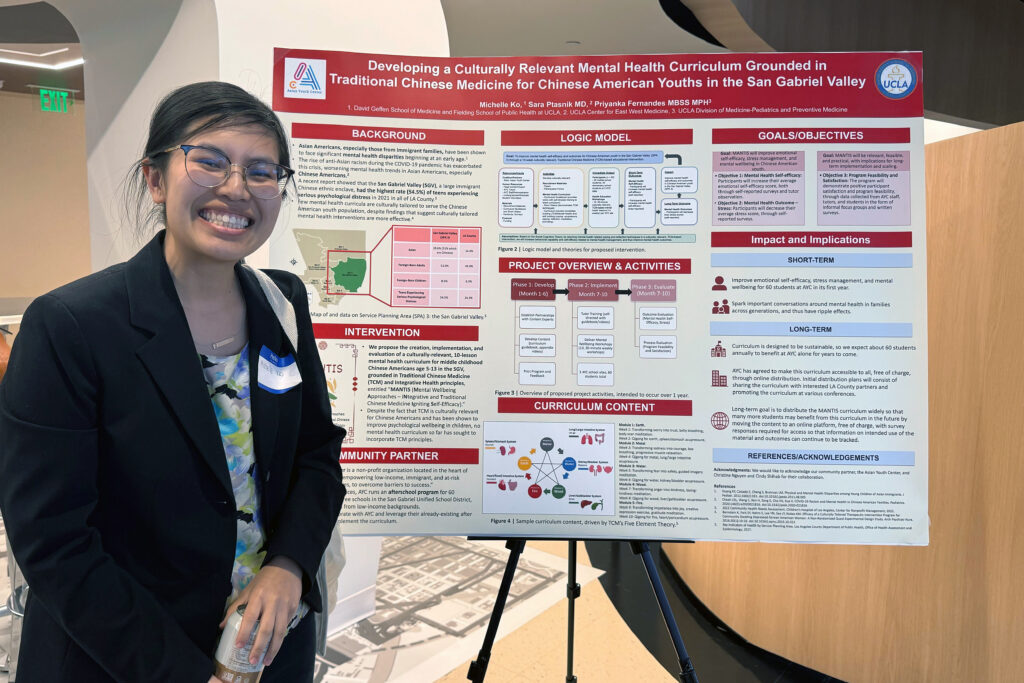
Community-based partner: Asian Youth Center
Michelle Ko’s project aims to create a mental health care curriculum that will integrate Traditional Chinese Medicine (TCM) with Integrative Health for youth ages 5 to 13 in Los Angeles County’s San Gabriel Valley.
A 2022 Community Health Needs Assessment by Children’s Hospital Los Angeles showed that the San Gabriel Valley had the highest rate (54.5%) of teens experiencing serious psychological distress in the past year in all of L.A. County. Potential contributing risk factors to such disparities include systemic issues such as barriers in access to care, racism and discrimination, and language barriers, as well as cultural issues such as culturally incongruent care and the stigmatization of mental health within several Asian cultures.
For Ko, focusing on culturally relevant mental health care is personal. “I’m originally from the San Gabriel Valley area and so that area is very near and dear to me and just from experience and from talking to a lot of folks in the community, I know that mental health is a big issue,” said Ko, who is a medical student at the David Geffen School of Medicine at UCLA and a Master of Public Health student at the UCLA Fielding School of Public Health.
Ko’s curriculum will empower youth by sparking conversations around and teaching self-efficacy techniques for mental health, using principles such as acupressure, journaling, meditation, and qigong.
“Though several general mental health curricula already exist, and though separate components of TCM have been used in an intervention setting to address mental health,” Ko wrote in her blog about the project, “to our knowledge this is the first that combines these components to create a comprehensive mental health curriculum for youth using TCM as a foundation.”
Spill the Chai Ma
Supraja Saravanakumar
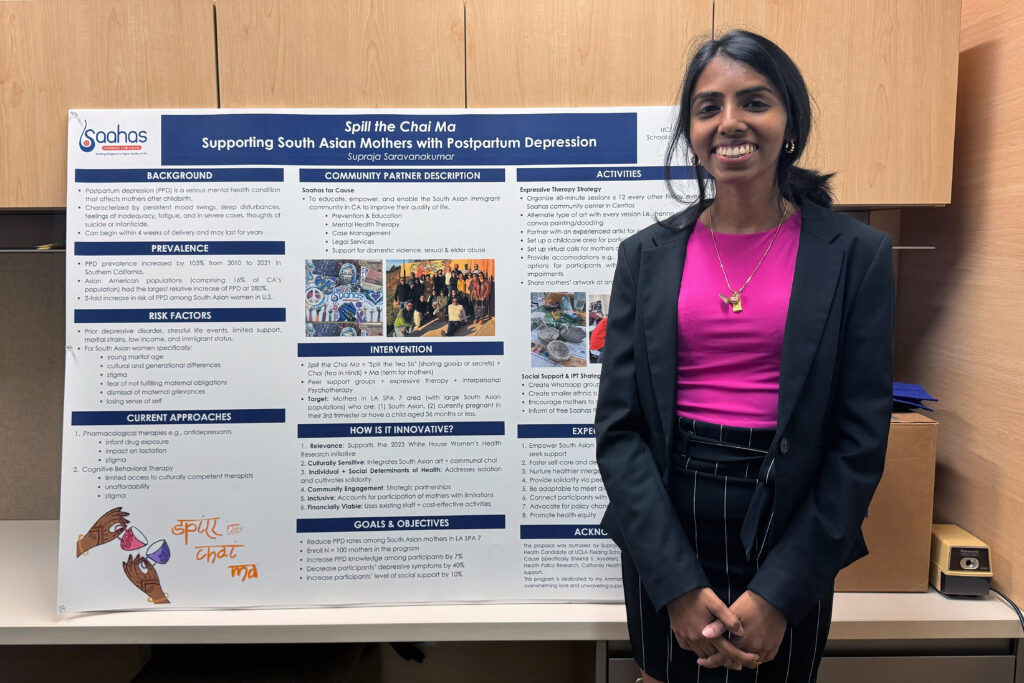
Community-based partner: Saahas for Cause
Supraja Saravanakumar’s project focuses on addressing postpartum depression among South Asian women in Los Angeles. Named “Spill the Chai Ma” to play off the phrase “spilling the tea,” the project is meant to offer an inviting atmosphere for women to talk about a serious health concern. To add to the welcoming environment, Spill the Chai Ma will also offer art therapy like henna, painting, and clay molding.
Saravanakumar said that as a South Asian woman this project was personal.
“I wanted to focus on mental health with the Health Equity Challenge, because that’s a topic that’s close to my heart. It’s close to challenges that my family has faced in the past,” said Saravanakumar, a Master of Public Health student in the department of Community Health Sciences at the UCLA Fielding School of Public Health.
“And there’s so much stigma around even just the label of mental health. There is literally no translation or interpretation of the word ‘mental health’ in a lot of South Asian languages.”
As Saravanakumar started shaping the idea her first sounding board wasn’t a fellow student or one of her professors, but instead it was her mom.
“I asked her, ‘What do you think we can do that you will actually use or participate in if you were to be in this position?’” Saravanakumar recalled. “And for her, it all came down to conversation. She wanted to talk about this topic with other people.”
Saravanakumar’s ammamma (grandmother) also played huge role.
“She passed away right before I started grad school and the reason was around mental health,” she said. “I have her photo in a locket that I wear on my neck. So right before they start announcing the winners, I just opened up the locket so she can just watch no matter what the results are because this was all inspired by her in a way.”